Electrophysiology is a branch of cardiology that focuses on the diagnosis and treatment of cardiac arrhythmias due to abnormalities in the heart’s electrical system.
Electrophysiologists, also known as Cardiac EPs are doctors of medicine who have specialized training and board certification in cardiology and cardiac electrophysiology.
What does electrophysiology treat?
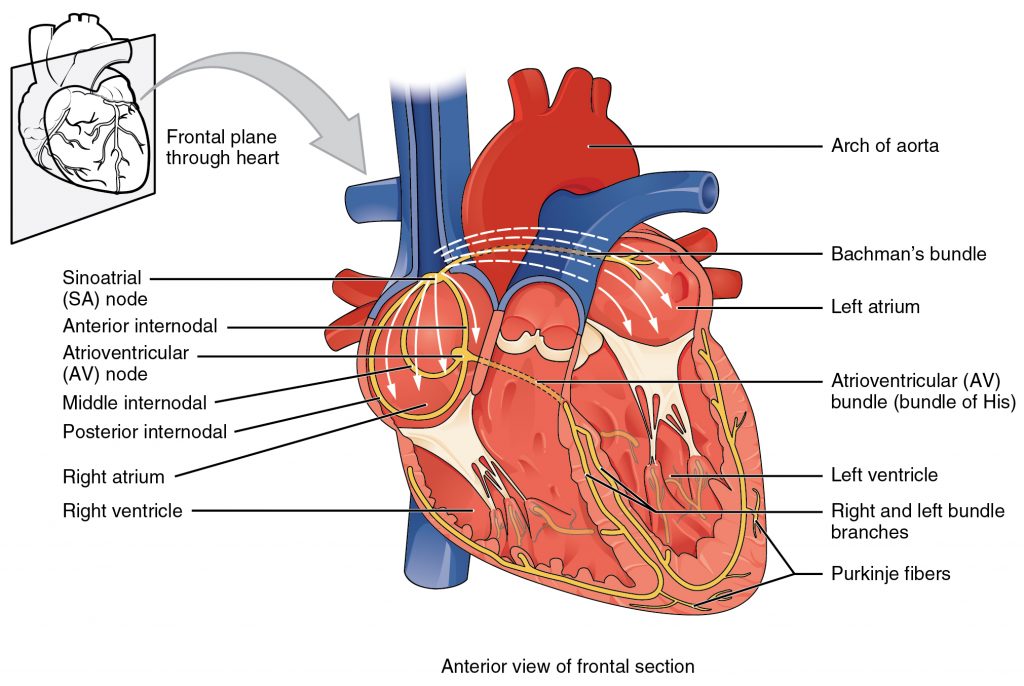
The field of electrophysiology is mainly concerned with the heart’s electrical system, or how the heart beats. The most common issues regarding the heart’s electrical system are abnormalities in the hearts rhythm, known as arrhythmias. Cardiac arrhythmias come in many different forms, including:
- Bradycardia: A slower than average resting heart rate. If your resting heart rate is under 50 beats per minute on a consistent basis, ask your primary care physician about bradycardia.
- Tachycardia: A faster than average resting heart rate. If your resting heart rate is over 100 beats per minute on a consistent basis, ask your primary care physician about tachycardia.
- Supraventricular tachycardia and ventricular tachycardia: Common types of Tachycardia. Supraventricular tachycardia occurs in the upper chambers of the heart while ventricular tachycardia occurs in the bottom chambers.
- Atrial Fibrillation: An irregular and fast heartbeat that manifests in the upper chambers of the heart. Atrial Fibrillation, commonly referred to as AFib, is the most common type of cardiac arrhythmia.
- Ventricular Fibrillation: A fluttering of the heart. Ventricular Fibrillation stops the heart from properly pumping blood.
- Cardiac Arrest: When the heart stops beating suddenly.
- WPW (Wolf-Parkinson-White) Syndrome: A condition where you are born with an extra electrical pathway to the heart, resulting in recurring episodes of fast heartbeat.
- Long QT Syndrome (LQTS): A condition that can cause frenzied, chaotic, and fast heartbeats.
These are just a few of the conditions that our electrophysiologists diagnose and treat on a daily basis.
How does the cardiac EP diagnose heart rhythm disorders?
First, the patient is seen in consultation. Information from the patient’s primary care physician (History and Physical, medication history, office notes, EKGs, lab work, imaging studies) are reviewed. The patient is interviewed and a physical exam is done to understand the patient’s symptoms and get clues on what the arrhythmia may be.
Initial testing ordered by the Cardiac EP to better characterize the arrhythmia may include:
- EKG or ECG (Electrocardiogram): A study that is conducted while the heart is in a resting state. An EKG records the electrical activity in the heart to detect arrhythmias.
- Holter Monitor: Records the heart’s electrical activity over a period of 24 hours or more to detect irregularities.
- Event Monitor: Records the heart’s rhythm over a long period of time when activated to detect irregularities.
- Exercise Stress Test: Detects abnormalities in the heart’s rhythm while the patient is exercising on a treadmill or stationary bike.
Further information concerning the heart’s structure and function that could influence arrhythmias may be needed from tests that could include cardiac echocardiography, cardiac CT scan, and/or cardiac MRI scan.
At this point, the Cardiac EP may have enough information to make a diagnosis as to what the arrhythmia is and then prescribe medication, device, or ablation.
Sometimes, the diagnosis is not clear and then an electrophysiological study (EP study) is performed in order to correctly diagnose the disorder.
What is an EP study?
An EP study records the electrical activity of your heart in a controlled setting. To record the electrical activity, thin wires are passed through a narrow tube into your heart. This process is not unlike cardiac catheterization. Doing this allows electrophysiologists to recreate arrhythmias safely.
How are cardiac arrhythmias treated?
Cardiac EPs may prescribe:
- Lifestyle changes: diet, relaxation techniques, and an exercise program may control fast heart rates
- Pacemaker: with a generator and leads may be inserted via a vein from the chest to the heart to regulate slow heart beats. Some pacemakers help the heart beat more efficiently through resynchronization therapy
- Implantable Cardioverter Defibrillator (ICD): may be placed similar to a pacemaker to stop rapid life threatening heart rhythms of the ventricle (ventricular fibrillation and ventricular tachycardia). Some ICDs also incorporate very sophisticated pacemakers also to resynchronize the heart beat and improve pumping efficiency.
- Catheter Ablation: Catheters are inserted through blood vessels and into the heart. Short circuits in the heart tissue that are causing fast heart rhythms are identified and then destroyed or isolated with radio frequency energy or freezing to prevent the fast heart rhythm from recurring.
Other services offered by our electrophysiologists
- Chronic Follow up for Device Patients: Patients with cardiac implantable electronic devices like pacemakers and ICDs need chronic follow up by a Cardiac EP. These devices record information about heart rhythm issues. This information is used by the Cardiac EP to optimize programmable settings in the device and to adjust medical therapy with the goal of improving the cardiac well being of the patient. Nearly all devices can now be implemented remotely which may cut down on office visits.
- Device Generator Change: pacemaker and ICD generators last 6 to 10 years before needing changeout. The Cardiac EP can do this in a simple outpatient procedure in several hours or less.
- Lead management: most ICDs and pacemakers utilize leads that are placed in a vein to the heart. Sometimes leads fail and have to be removed. The Cardiac EP can remove old leads using laser lead extraction.
- Left Atrial Appendage Occlusion: the left atrial appendage is the source of most of the blood clots that can cause stroke in atrial fibrillation. Clots are usually treated and prevented with blood thinners. Some patients are not candidates for blood thinners. They may qualify for a device like Watchman that can be inserted via a vein into the left atrial appendage to prevent clots from forming there
What are electrophysiologists?
Electrophysiologists are cardiologists who have a special interest, as well as have undergone extensive training, in abnormalities of the heart’s electrical system. To become an electrophysiologist, you must complete undergraduate school (3-4 years), medical school (4 years), an internal medicine residency (3 years), and a cardiology fellowship (3 years). They must then pass an exam from the American Board of Internal Medicine to become board-certified in cardiovascular disease. Afterwards, an additional 2 years of training in electrophysiology must be completed.