Peripheral vascular disease (PVD) is an umbrella term for diseases and disorders of blood vessels outside of the heart. It is commonly found in vessels inside the brain, kidney, stomach, and limbs. PVD decreases blood circulation in the body, causing pain and fatigue in affected areas.
PVD that specifically affects the arteries is called peripheral arterial disease, or PAD. PAD is the most common form of PVD. Approximately 12 to 20% of all Americans over the age of 60 suffer from PAD.
What causes PVD?
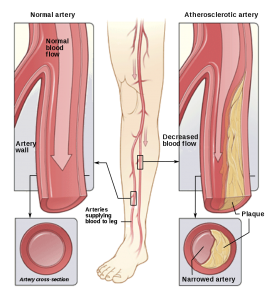
The decreased blood circulation in PVD is most often caused by atherosclerosis, the hardening of the arteries, or blood vessel spasms. Atherosclerosis occurs when plaque coagulates in a blood vessel or artery; blocking, or severely inhibiting, blood flow through the passageway.
When blood flow is blocked or reduced by plaque, blood clots may form against the artery or vessel wall, causing further damage to the passageway. Atherosclerosis may also lead to coronary artery disease.
While PVD is an umbrella term, it can be divided into two categories depending on the causes.
Functional PVD is when your surrounding environment can be attributed as a cause. Blood vessels contract and expand in response to what the body is doing or going through. In functional PVD, the vessels are overestimating their response. Operating certain types of machinery, going through high levels of emotional stress, being exposed to cold temperatures, or using certain drugs may cause functional PVD.
Organic PVD is when a physical change to the blood vessel or artery occurs. Plaque buildup (atherosclerosis) is a common symptom of organic PVD. Consistent smoking, high blood pressure and/or cholesterol, and diabetes may cause organic PVD.
What are common symptoms of PVD?
You may not notice any symptoms of PVD at first, as many of its symptoms can be attributed to the normal aging process. However, symptoms may develop and cause serious complications. Ask your doctor if you experience any of the following:
- Muscle pain and fatigue in your lower extremities while walking. This is known as claudication.
- A noticeable lack of hair growth in your legs
- Slow healing injuries
- A numb or “heavy” feeling in your muscles
- A change of coloring (usually to a purple-like color) in your extremities
- A bluish tinge in your toes.
While PVD is a slow forming disease, diagnosis and treatment at an early stage reduces the chance of serious issues. Gangrene and dead tissue may form in cases of serious blood loss. If you notice a sudden pain, loss of color, and lack of a pulse in one of your limbs, please call a medical emergency number or 911. This issue is a medical emergency and must be treated as soon as possible to avoid amputation.
How is PVD treated?
There has been a paradigm shift in the way PAD is now treated. While earlier the only way to treat blockages in the arteries was by doing surgeries. Now our doctors can do that by minimally invasive procedures like angioplasty, stents and atherectomy.
Your doctor may prescribe other treatments and lifestyle changes to stop the disease from progressing. These lifestyle changes may include:
- A regular exercise program to stimulate blood flow.
- A new diet that is more balanced than your current one.
- A weight loss program if you are overweight.
- Quitting smoking if you smoke.
To prevent PVD, consider implementing the above lifestyle changes as soon as possible. Even making small changes to your lifestyle, such as walking for 30 minutes a day, may greatly reduce the risk of PVD.
Aside from lifestyle modifications, your doctor may prescribe certain medications to help you manage PVD. These medications are prescribed to help you:
- Increase blood flow
- Stop the progression of claudication
- Reduce blood clotting
- Lower high cholesterol
- Control blood sugar
Arteries take blood to the feet while veins return blood to the heart. Interruption in the process of normal blood flow through the veins can have serious consequences. Without treatment, a minor problem with your veins can get much worse. So, it’s important to see a doctor, whether to treat a potentially life-threatening condition, such as preventing blood clots in the deep veins, or to find relief from swelling, pain, and sores.
Your doctor may recommend some things you can do on your own to treat the problem and prevent more serious conditions. Or, if something more serious is suspected, your doctor might refer you to someone who specializes in treating more serious vein problems.
Types of treatment for leg vein problems
- Lifestyle Changes – Lose weight, exercise, and move your feet and legs if sitting for a long time, for example, sitting at your desk or traveling.
- Home Care – Compression stockings, leg elevation, warm moist compresses and rest.
- Medications – Anticoagulants (blood thinners) to reduce the risk of clots getting bigger and the development of new clots. Anti-inflammatory drugs such as ibuprofen to reduce pain and swelling.
- Interventional procedures – If the deep venous system (large veins) is blocked, leg swelling and discomfort may become severe. This can happen suddenly when a blood clot (DVT) forms and closes off blood flow or more gradually when pressure outside the vein in the pelvis presses onto and obstructs the large pelvic veins. In some cases, the patient needs to be hospitalized when a thrombolytic (clot busting medication) is required to dissolve clots.
In other cases, an outpatient procedure is performed where a small balloon or stent is inserted into the vein that will open it wider and keep it open. This allows blood to flow more freely through the vein. After blood is flowing freely the symptoms begin to improve.